Alzheimer's and Elder Care
You’re Looking at Me Like I Live Here and I Don’t
Independent Lens
by Scott Kirschenbaum
In Danville, California, the Traditions Alzheimer’s Care Unit houses 20 residents who are shepherded by caregivers through scheduled activities like balloon baseball and
bingo. For most residents, life is routine.
But for Lee Gorewitz, life is an odyssey.
From the moment she wakes up, Lee is on a quest for something that she can neither articulate nor comprehend. Confined by the physical boundaries of the Care Unit, she
scavenges for reminders of her past identity.
A total immersion into the fragmented day-to-day experience of Alzheimer’s disease, You’re Looking at Me Like I Live Here and I Don’t is the first documentary filmed
exclusively in an Alzheimer’s care unit, told from the perspective of someone suffering from the disease. Read more
You’re Looking at Me Like I Live Here and I Don’t, Facebook
Unflinching View of a Wandering Mind, No Breadcrumb Trail in
Sight
The New York Times
By NEIL GENZLINGER
March 28, 2012
Perhaps years from now, after a scientific breakthrough has turned Alzheimer’s disease into a memory as distant as polio wards are to younger Americans today, someone
will stumble upon Scott Kirschenbaum’s hard-to-watch documentary, "You’re Looking at Me Like I Live Here and I Don’t," and be stunned. "I’ve read about Alzheimer’s," this person will say, "but I had
no idea what it was actually like."
Alzheimer’s has been a trendy topic for writers of plays and television scripts in recent years. But those stories have often been primarily about the people surrounding
the patient — family members, friends — and the effect of the disease on their lives.
Mr. Kirschenbaum, whose film will be broadcast
nationally on PBS’s "Independent Lens" on Thursday (on Sunday on Channel 13 in New York), takes the simple but bold step of making Alzheimer’s the only thing in his tale. It’s not a plot point that propels a
narrative; it’s an inescapable box. Read more
The Alzheimer's Project - HBO documentary
One of the most devastating forms of memory loss is Alzheimer's disease, an irreversible and progressive brain disorder that slowly destroys memory and thinking skills.
Today, Alzheimer's is the second most-feared illness in America, following cancer, and may affect as many as five million Americans. As the baby-boom generation moves through retirement, that number
could soar to more than 11 million by 2040, and have a huge economic impact on America's already fragile healthcare system. Read more
______________________________________
Aging In Place - Guide To Recognizing Elder Abuse
_______________________________________
Alzheimer's disease
From Wikipedia, the free encyclopedia
Left: Alzheimer’s Awareness
Commemorative Stamp, USPS
Alzheimer's disease (AD), also called Alzheimer disease, senile dementia of the Alzheimer type, primary degenerative dementia of the Alzheimer's type, or simply
Alzheimer's, is the most common form of dementia. This incurable, degenerative, and terminal disease was first described by German psychiatrist and neuropathologist Alois Alzheimer in 1906 and was
named after him. Most often, it is diagnosed in people over 65 years of age, although the less-prevalent early-onset Alzheimer's can occur much earlier. In 2006, there were 26.6 million sufferers
worldwide. Alzheimer's is predicted to affect 1 in 85 people globally by 2050.
Although the course of Alzheimer's disease is unique for every individual, there are many common symptoms. The earliest observable symptoms are often mistakenly thought to be 'age-related' concerns,
or manifestations of stress. In the early stages, the most commonly recognised symptom is inability to acquire new memories, such as difficulty in recalling recently observed facts. When AD is
suspected, the diagnosis is usually confirmed with behavioural assessments and cognitive tests, often followed by a brain scan if available. Read more
______________________________________
Aging In Place - Guide To Recognizing Elder Abuse
_______________________________________
New guidelines define pre-Alzheimer's disease
By MARILYNN MARCHIONE
AP Medical Writer
April 20, 2011
The first new guidelines for diagnosing Alzheimer's disease in nearly 30 years establish earlier stages of the mind-robbing disease, paving the way for spotting and possibly treating these conditions
much sooner than they are now.
The change reflects a modern view that Alzheimer's is a spectrum of mental decline, with damage that can start many years before symptoms appear. The new guidance describes three phases: early brain
changes, mild cognitive impairment and full-blown Alzheimer's.
Yet the guidelines do not advise doctors to change how they evaluate and treat patients now. Despite the hoopla about new brain scans and blood and spinal fluid tests
that claim to show early signs of Alzheimer's, they are not ready for prime time and should remain just tools for research, the guidelines say.
"It's too soon right now" to say these experimental biomarker tests will prove valid enough to be used in ordinary patient care, said Creighton Phelps, Alzheimer's program chief at the National
Institute on Aging.
His institute and the Alzheimer's Association convened several expert panels to write the guidelines, the first since 1984. They are being published Tuesday in Alzheimer's & Dementia: The Journal
of the Alzheimer's Association.
About 5.4 million Americans and more than 26 million people worldwide have Alzheimer's, the most common form of dementia.
Primary Federal Agency on Alzheimer’s Disease Research
NIA, one of the 27 Institutes and Centers of National
Institutes of Health (NIH), leads a broad scientific effort to understand the nature of aging and to extend the healthy, active years of life. In 1974, Congress
granted authority to form NIA to provide leadership in aging research, training, health information dissemination, and other programs relevant to aging and older people. Subsequent amendments to this
legislation designated the NIA as the primary Federal agency on Alzheimer’s disease research. Read more
NIA: Coping with Emotions and Stress in
Alzheimer’s Caregiving: A Resource List
NIA 2009 Progress Report on Alzheimer’s Disease
2009 Progress Report on Alzheimer’s Disease: Translating New Knowledge
The National Institute on Aging (NIA), part of the Federal Government's National Institutes of Health (NIH) at the U.S. Department of Health and Human Services, has
primary responsibility for basic, clinical, behavioral, and social research in Alzheimer's disease (AD), aimed at finding ways to treat and, ultimately, prevent this disease. The Institute's AD
research program is integral to its mission, which is to enhance the health and well-being of older people. This 2009 Progress Report on Alzheimer's Disease summarizes recent AD research conducted or
supported by NIA and other components of NIH. Read more
2009ADProgressReportFinalB.pdf
Adobe Acrobat document [2.1 MB]
Aging in Place is a resource hub for seniors and their families to learn more about the specific aspects of aging in place. You can visit our one stop shop for expert know-how in order to make the best decisions about in-home care, insurance, government assistance, and other financial resources, transportation options, and home remodeling.
Legal Services for the Elderly (Title III-B) provides legal assistance nationwide on issues such as income security, healthcare, long-term care, nutrition, housing, utilities, protective services, defense of guardianship, abuse, neglect, and age discrimination. This assistance is targeted towards older individuals in social and economic need.
Legal Services for the Elderly Program
Authorizing Legislation: Title III-B, Section 321, of the
Older Americans Act, as amended
The Purpose of the Program and How it Works
Legal assistance provided under Title III-B is part of the essential core of AoA’s legal assistance and elder rights programs. The legal services network can provide important assistance for older persons in accessing long-term care options and other community-based services. Legal services also protect older persons against direct challenges to their independence, choice, and financial security. These legal services are specifically targeted to "older individuals with economic or social needs."
There are approximately 1,000 OAA-funded legal services providers nationwide, which provide nearly one million hours of legal assistance each year. Legal assistance provided may involve:
- Access to public benefits, including SS/SSI/SSDI, Medicaid and Medicare, veterans benefits, and unemployment compensation;
- Drafting advance directives and designating surrogate decision makers who will effectuate older adults' wishes if they become incapacitated;
- Issues related to guardianship with a focus on representation for older persons who are the subject of guardianship actions;
- Access to available housing options, including low income housing programs that allow independence in homes and communities;
- Foreclosure or eviction proceedings that jeopardize the ability to stay independent in homes and communities;
- Gaining access to the full benefit of appropriate long-term care private financing options;
- Maintaining long-term financial solvency and economic security;
- Ensuring elder rights protections for older persons transferring from long-term care facilities to home and community-based care; and
- Elder abuse, including consumer fraud and the financial exploitation of older persons.
The legal assistance provided to thousands of older persons each year has a clear and direct positive impact on their ability to stay independent in their homes and communities, with optimized choice and individual autonomy, for as long as possible. The following examples demonstrate the benefits: Read more
The National Center on Law and Elder Rights serves as a centralized access point for a national
legal assistance support system serving professionals and advocates working in legal and aging services networks. Read
more
_____________________________________________
Florida Department of Elder Affairs
_____________________________________________
The Florida Department of Elder Affairs is the primary state agency administering human services programs to benefit Florida’s large and growing elder population. Whether you are an elder or caregiver, a professional or volunteer who deals with aging issues, or just looking for information related to Florida’s older residents, this website is a valuable tool for you.
2016 Summary of Programs and Services
This document is produced by the Florida Department of Elder Affairs and updated periodically to provide the public and the Legislature with information about programs
and services for Florida’s elders. Services and programs for elders vary in relation to consumer needs, demographics, funding availability and legislative directives. This Summary of Programs and
Services, unless otherwise noted, contains information and data compiled as of September 2015.
Link to all Florida Dept. of Elder Affairs Programs and Services
- Alzheimer’s Disease Initiative (ADI)
- RELIEF (Respite for Elders Living in Everyday Families)
- Program of All-Inclusive Care for the Elderly (PACE)
- Home Care for the Elderly (HCE)
Department of Elder Affairs' Office of Legislative Affairs
Here you will find updated information on legislative action taking place within the Florida Legislature. Also listed:
- Annual Reports Required by Statute
- Annual Reports to the Legislature
- Presentations
- Budgetary Information
- End of Legislative Session Reports
- Links to Important Websites and Statutes
Archival information below
2009 Memory Disorder Clinics and Brain B[...]
Adobe Acrobat document [2.4 MB]
Memory Disorder Clinics, 2008 Year End S[...]
Adobe Acrobat document [700.6 KB]
Alzheimers Disease Advisory Committee 20[...]
Adobe Acrobat document [247.6 KB]
Hospice Demographic and Outcomes Measure[...]
Adobe Acrobat document [305.7 KB]
2009 Division Community Services Monitor[...]
Adobe Acrobat document [11.5 MB]
2009 CARES Diversions Report.pdf
Adobe Acrobat document [357.8 KB]
2009 Long-Term Care Community Diversion [...]
Adobe Acrobat document [433.7 KB]
2009 Extended Congregate Care Annual Rep[...]
Adobe Acrobat document [423.7 KB]
2010 Legislative Action Summary.pdf
Adobe Acrobat document [268.1 KB]
DOEASchedule8BNovember2009.pdf
Adobe Acrobat document [368.3 KB]
Statewide Public Guardianship Office (SPGO)
Generally, there are three types of guardians in Florida. If a court determines a person needs a guardian and that person has family or friends who can serve, then the court may appoint that family
or friend. These people are considered non-professional guardians. If the incapacitated person does not have a loved one who can and will serve, but they have assets, the court may appoint a
professional guardian to be paid from the person’s assets. If the incapacitated person does not have family or friends and is of limited financial means, then the court may appoint a public guardian,
if available.
2009 Statewide Public Guardianship Offic[...]
Adobe Acrobat document [1.2 MB]
SPGO anual report 2008 WebVersion.pdf
Adobe Acrobat document [573.6 KB]
..............................Florida Senior Fact Sheet...........................
24/7 Helpline: 1.800.272.3900
The Alzheimer's Association is the leading, global voluntary health organization in Alzheimer care and support, and the largest private, nonprofit funder of Alzheimer
research.
In 1979, Jerome H. Stone and representatives from several family support groups met with the National Institute on Aging to explore the value of a national, independent, nonprofit organization to
complement federal efforts surrounding Alzheimer's disease. That meeting resulted in the April 10, 1980, formation of the Alzheimer's Association with Mr. Stone as founding president.
Today, the Association reaches millions of people affected by Alzheimer’s across the globe through our national office and more than 75 local chapters. As the largest donor-supported, voluntary
health organization for Alzheimer’s, the Association is a catalyst for advancements in Alzheimer research and care.
Alzheimer's Association National Office 225 N. Michigan Ave., Fl. 17, Chicago, IL 60601. Alzheimer's Association is a not-for-profit 501(c)(3) organization
Experts have developed "stages" to describe how a person's abilities change from normal function through advanced Alzheimer's. It is important to keep in mind that stages are general guides, and symptoms vary greatly. Not everyone will experience the same symptoms or progress at the same rate. This seven-stage framework is based on a system developed by Barry Reisberg, M.D., clinical director of the New York University School of Medicine's Silberstein Aging and Dementia Research Center.
______________________________________
Aging In Place - Guide To Recognizing Elder Abuse
_______________________________________
The Spiritual Implications of Dementia
The Huffington Post
by Lynn Casteel Harper
July 13, 2010
Ordained Baptist minister and retirement community chaplain
The morning my grandmother suffered her life-ending stroke, my grandfather, after trying to rouse his wife of 65 years, went outside and mowed the lawn. On the
morning of her funeral, he refused to shower. A few days later, passing by her picture, he stated, "I haven't seen that woman in a while."
He wasn't calloused; he was confused.
My grandfather is among the millions of people who have dementia, and my grandmother was one of the many family caregivers who predecease their sick partners. I am among the growing number of
intimate bystanders who know and love someone with dementia. I also happen to work in a skilled nursing facility as the chaplain to many residents with some form of dementia.
Eloquence is irrelevant: dementia sucks really bad. Dementia defies platitudes and niceties; however, it does not defy meaning and life.
The truth is, we are all one tick away from terror and triumph, from exultation and annihilation. In a nanosecond, your carefully calculated savings can be multiplied or drained, your health
decimated or restored. Read more
Link to Alzheimer’s related articles and videos from the New York Times
Alzheimer’s Caregiver Handbook Accessible Home Health Care
PTSD Linked to Dementia
By Todd Neale, Staff Writer, MedPage Today
Published: June 07, 2010
Reviewed by Robert Jasmer, MD; Associate Clinical Professor of Medicine, University of California, San Francisco and Dorothy Caputo, MA, RN, BC-ADM, CDE, Nurse Planner
Older U.S. veterans with post-traumatic stress disorder (PTSD) appear to have an increased risk of developing dementia, a retrospective study showed.
Compared with those without PTSD, predominantly male veterans with the disorder had a 1.77-fold (95% CI 1.70 to 1.85) greater risk of developing dementia, according
to Kristine Yaffe, MD, of the San Francisco Veterans Affairs Medical Center and the University of California San Francisco, and colleagues.
The results were similar when veterans with a history of head injury, substance abuse, and clinical depression were excluded, the researchers reported in the June issue of Archives of General
Psychiatry.
"It is important that those with PTSD are treated, and further investigation is needed to see whether successful treatment of PTSD may reduce the risk of adverse health outcomes, including dementia,"
Yaffe and her colleagues wrote.
"In addition, it is critical to follow up patients with PTSD, especially if they are of an advanced age, to screen for cognitive impairment."
PTSD is common among U.S. veterans, affecting an estimated 17% of soldiers returning from Iraq and Afghanistan. The disorder can persist for decades.
There is some evidence of a link between PTSD and impaired cognition, although little is known about PTSD's potential as a
risk factor for dementia. Read more
Hallucinations in Hospital Pose Risk to the Elderly
The New York Times
By PAM BELLUCK
June 20, 2010
No one who knows Justin Kaplan would ever have expected this. A Pulitzer Prize-winning historian with a razor intellect, Mr. Kaplan, 84, became profoundly delirious while hospitalized for pneumonia
last year. For hours in the hospital, he said, he imagined despotic aliens, and he struck a nurse and threatened to kill his wife and daughter.
"Thousands of tiny little creatures," he said, "some on horseback, waving arms, carrying weapons like some grand Renaissance battle," were trying to turn people "into
zombies." Their leader was a woman "with no mouth but a very precisely cut hole in her throat."
Attacking the group’s "television production studio," Mr. Kaplan fell from his hospital bed, cutting himself and "sliding across the floor on my own blood," he said. The hospital called security
because "a nurse was trying to restrain me and I repaid her with a kick."
Mr. Kaplan’s hallucinations lifted as doctors treated his pneumonia. But hospitals say many patients are experiencing such inexplicable disorienting episodes. Doctors call it "hospital delirium," and
are increasingly trying to prevent or treat it. Read more
Wife of early-onset Alzheimer's patient haunted by handcuffs
The Roanoke Times
by Beth Macy
August 9, 2009
Steve Ward, shown here with one of his pets, died at age 60 of end-stage Alzheimer's disease. Reports prepared for Gov. Tim Kaine and the General Assembly in 2006 and 2007 said that on any given
day, regional and local jails in Virginia care for 60 percent of the state's mentally ill people.
It's not just the absence of Steven Ward that his widow, Gail, has struggled with since his death nine months ago. It wasn't even his diagnosis of Alzheimer's disease
-- at the shockingly young age of 56.
Gail Ward, 58, has been a long-term care nurse for decades and knows the struggles of caring for demented patients well.
No, the memory that haunts the Roanoke woman is of her fearful, confused husband being escorted into an emergency commitment hearing -- in handcuffs and shackles -- and pleading with her to tell him:
"What did I do wrong?"
Gail Ward, standing in front of a photo collection of her husband, says Steven Ward was diagnosed with Alzheimer's disease at the young age of 56, and she had to struggle to find appropriate care for him. Steve died in November.
He did nothing wrong -- intentionally -- but his behavior proved to be a challenge for the area's medical and legal systems. It's a story that will not go away with
Steve Ward's passing, not with 6 million baby boomers shuffling toward retirement.
In the Roanoke region alone, a projected 13,666 people will have Alzheimer's by 2030. At least half will at some point display the kind of violent behavior Steve Ward showed the night he was hauled
away by police from his room at The Court, an assisted living facility for Alzheimer's patients in Roanoke.
Gail Ward worries: If a veteran long-term care nurse can't navigate the medical, financial and legal maze laid out before caregivers of people with Alzheimer's, how will the rest of us manage?
more
Doctor says an oil lessened Alzheimer's effects on her
husband
Tampa Bay Times
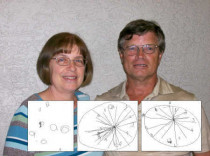
by Eve Hosley-Moore, Times Correspondent
October 29, 2008
After two weeks of taking coconut oil, Steve Newport's results in an early onset Alzheimer's test gradually improved says his wife, Dr. Mary Newport. Before treatment,
Steve could barely remember how to draw a clock. Two weeks after adding coconut oil to his diet, his drawing improved. After 37 days, Steve's drawing gained even more clarity. The oil seemed to "lift
the fog," his wife says. Read more
Hard Choice for a Comfortable Death: Sedation
The New York Times
by Anemona Hartocollis
December 26, 2009
Left: Frank Foster, sleeping under sedation to relieve pain and other effects of liver cancer, at a Long Island hospice unit.
In almost every room people were sleeping, but not like babies. This was not the carefree sleep that would restore them to rise and shine for another day. It was the
sleep before - and sometimes until - death.
In some of the rooms in the hospice unit at Franklin Hospital, in Valley Stream on Long Island, the patients were sleeping because their organs were shutting down, the
natural process of death by disease. But at least one patient had been rendered unconscious by strong drugs.
The patient, Leo Oltzik, an 88-year-old man with dementia, congestive heart failure and kidney problems, was brought from home by his wife and son, who were distressed to see him agitated, jumping
out of bed and ripping off his clothes. Now he was sleeping soundly with his mouth wide open.
"Obviously, he’s much different than he was when he came in," Dr. Edward Halbridge, the hospice medical director, told Mr. Oltzik’s wife. "He’s calm, he’s quiet."
Left: Barbara Walsh, a nurse on the hospice unit at Franklin Hospital, and Dr. Edward Halbridge are part of a team that works with patients and their families to map out end-of-life care.
Mr. Oltzik’s life would end not with a bang, but with the drip, drip, drip of an IV drug that put him into a slumber from which he would never awaken. That drug,
lorazepam, is a strong sedative. Mr. Oltzik was also receiving morphine, to kill pain. This combination can slow breathing and heart rate, and may make it impossible for the patient to eat or drink.
In so doing, it can hasten death.
Mr. Oltzik received what some doctors call palliative sedation and others less euphemistically call terminal sedation. While the national health coverage debate has been roiled by questions of
whether the government should be paying for end-of-life counseling, physicians like Dr. Halbridge, in consultations with patients or their families, are routinely making tough decisions about the
best way to die.
Among those choices is terminal sedation, a treatment that is already widely used, even as it vexes families and a profession whose paramount rule is to do no harm.
Doctors who perform it say it is based on carefully thought-out ethical principles in which the goal is never to end someone’s life, but only to make the patient more comfortable.
But the possibility that the process might speed death has some experts contending that the practice is, in the words of one much-debated paper, a form of "slow euthanasia," and that doctors who say
otherwise are fooling themselves and their patients. Read more
Family Caregiver Alliance
Family Caregiver Alliance was the first community-based nonprofit organization in the country to address the needs of families and friends providing long-term care at home. Long recognized as a pioneer in health services, FCA now offers programs at national, state and local levels to support and sustain caregivers.
More than 30 years ago, a small task force of families and community leaders in San Francisco came together to create support services for those struggling to provide long term care for a loved one who did not "fit" into traditional health systems: adults suffering from Alzheimer's disease, stroke, Parkinson's, traumatic brain injury and other debilitating disorders. The diagnoses were different, but the families shared common challenges: isolation, lack of information, few community resources, and drastic changes in family roles. Read more
Hospice
Wikipedia
Hospice is a type of care and a philosophy of care that focuses on the palliation of a terminally ill patient's symptoms. These symptoms can be physical, emotional,
spiritual or social in nature. The concept of hospice has been evolving since the 11th century. Then, and for centuries thereafter, hospices were places of hospitality for the sick, wounded, or
dying, as well as those for travelers and pilgrims. The modern concept of hospice includes palliative care for the incurably ill given in such institutions as hospitals or nursing homes, but also
care provided to those who would rather die in their own homes. It began to emerge in the 17th century, but many of the foundational principles by which modern hospice services operate were pioneered
in the 1950s by Dame Cicely Saunders. Although the movement has met with some resistance, hospice has rapidly expanded through the United Kingdom, the United States and elsewhere.
Read more
A free collection of articles about hospice care published in the NYT
______________________________________
Aging In Place - Guide To Recognizing Elder Abuse
_______________________________________
Hospice Foundation of America provides leadership in the development and application of hospice and its philosophy of care with the goal of enhancing the U.S. health care system and the role of hospice within it. Read more
Understanding Grief. If you have recently experienced the end of a caring relationship, you likely are experiencing grief. This program can help you understand what you may be feeling and why. It also offers some tips that may make grieving a little less painful.
Grief and Bereavement
Wikipedia
The family of the Alzheimer’s person may grieve the loss of their loved one’s mind, followed by a period of bereavement when the person dies. While the terms are often used interchangeably, bereavement often refers to the state of loss, and grief to the reaction to loss. Grief counseling is a form of psychotherapy that aims to help people cope with grief and mourning following the death of loved ones, or with major life changes that trigger feelings of grief.
On Death and Dying - The late Elisabeth Kubler-Ross, M.D. was a pioneer in Near-death studies and the author of the groundbreaking book On Death and Dying (1969), where she first discussed what is now known as the Kubler-Ross model.
The Elisabeth Kubler-Ross Foundation
Elisabeth Kubler-Ross Foundation is dedicated to furthering the legacy and work of pioneering legend, Dr. Elisabeth Kubler-Ross. Elisabeth Kubler-Ross is considered one
of the most influential people and important minds of the last century. Her personal grit and determination forever changed how the world treats its dying. Her tireless efforts to assure that those
who are dying be treated with compassion and dignity have now become the standard in end of life care. Dr. Ross taught the world that dying was actually about living and that our work here was to
learn how to love unconditionally. Read more
Dedication
This page is dedicated to my Mother Penny who died of Alzheimer’s disease. From 2005 through early 2009 I was Penny’s caregiver. The advice given here is from that
labor of love.
If I were to write a layman’s book on Alzheimer’s care, it would take a different approach from the Alzheimer’s books I have read. The first chapter would state the obvious but inescapable truth that
the patient never survives, no matter how excellent the care or how brilliant the physician. Unlike other illnesses, with Alzheimer’s there is no hope of recovery. This runs counter to the normal
human instinct of optimism.
The caregiver needs help before he or she realizes. I liken it to being outdoors in the summer heat, you need water before you feel thirst; by then you are probably dehydrated and at risk of heatstroke. Likewise for caregivers and respite. The caregiver needs help long before it is obvious. By then the caregiver is at risk of exhaustion and compromised ability to make good decisions.
Alzheimer’s presents illusions to the patient that can be traps to the caregiver. While sitting in her home of 16 years, my Mother frequently asked when she was going home. It would appear that since she did not recognize her home she would not know the difference living in my brother’s home far away in Texas. Not so. It only added to the already present confusion. Our small Florida retirement home was more senior friendly than his sprawling Texas executive home.
This seems obvious to me now, but in early 2009 I was too exhausted to realize. For this reason it is helpful for the caregiver to have another person as a confidant, not a family member, but someone who shares your values and whom has been a caregiver themselves. See the Family Caregiver Alliance.
My advice to caregivers would be get help early and often. Two hour respite visits by well-meaning church members are not enough. In our case isolation was a problem. Our nearest relatives are over a thousand miles away. I found a local home healthcare lady to help. The cost for such help starts at about $15 per hour. Forty hours of home healthcare a week, say 9am to 5pm for five days, would cost $320 at that rate. Round the clock home health care would cost over $10,000 a month.
There are programs to help pay the cost of eldercare if the person or spouse served in the military during war time. And Medicare offers a number of excellent publications vital to understanding home health care, nursing home facilities, and hospice services.
Do not ask me to remember.
Don’t try to make me understand.
Let me rest and know you’re with me.
Kiss my cheek and hold my hand.
I’m confused beyond your concept.
I am sad and sick and lost.
All I know is that I need you
To be with me at all costs.
Do not lose your patience with me.
Do not scold or curse or cry.
I can’t help the way I’m acting.
Can’t be different though I try.
Just remember that I need you,
That the best of me is gone.
Please don’t fail to stand beside me,
Love me ’til my life is done.
-Author unknown
Veterans Administration (VA) pension programs
The Veterans Administration offers pension programs, including Aid & Attendance, and Housebound benefits. My Mother was eligible for cash benefits of over $1,000 per month as a
surviving spouse of an eligible veteran. VA pension program information is online at
Unfortunately we were not aware of the VA pension program until shortly before Mom's death. We lost years of benefits that could have made a difference in her life.
Apparently this is not unusual.
VeteranAid.org and Debbie Burak, Founder
Left: Combat boots displayed in the Capitol Rotunda March, 2008 as part of the five-year anniversary of the Iraq War as part of the exhibit "Empty Boots: The Cost of War." Each pair represents a military member who has died in combat in Iraq and Afghanistan.
From the website: The Veterans Administration offers Aid and Attendance as part of an
"Improved Pension" Benefit that is largely unknown. This Improved Pension allows for Veterans and surviving spouses who require the regular attendance of another person to assist in eating, bathing,
dressing, undressing, medication dosing, or taking care of the needs of nature to receive additional monetary benefits. It also includes individuals who are blind or a patient in a nursing home
because of mental or physical incapacity. Assisted care in an Assisted Living facility also qualifies.
This most important benefit is overlooked by many families with Veterans or surviving spouses who need additional monies to help care for ailing parents or loved ones. This is a "Pension Benefit" and IS NOT dependent upon service-related injuries for compensation. Aid and Attendance can help pay for care in the home, Nursing Home or Assisted Living facility. A Veteran is eligible for up to $1,632 per month, while a surviving spouse is eligible for up to $1,055 per month. A couple is eligible for up to $1,949 per month*. Read more
Veteran Aid Facebook
Read the letter below in PDF from Debbie Burak about the delay in receiving VA benefits that inspired her to create VeteranAid.org
The Story of VeteranAid.org.pdf
Adobe Acrobat document [12.0 KB]
There is another intangible benefit of VA pension benefits, it gives families "permission" to employ home healthcare to help the person who needs assistance with bathing, feeding, and dressing. Sometimes family members are resistant to employ others to help at home, viewing it untoward since they believe it is their duty. This approach can fail due to the amount of work involved. A pension payment by the VA for that purpose can legitimize the expense. It also acknowledges the service to our country provided by the veteran and is an earned benefit, not welfare.
Leeza Gibbons Takes on Alzheimer’s
Leeza's Place is "A Place for Family Caregivers" is a community gathering place and resource center committed to
providing free support services, resources and programs for family caregivers taking care of a loved one with a memory disorder or any chronic and/or progressive illness.
Life doesn't always go as planned. The people we love get sick, they get diseases and we often feel helpless to do anything about it. When you are a husband or wife, son
or daughter, brother, sister or friend who takes care of someone in your family or someone you love, chances are you need help too. That's where we come in...
Leeza's Place is simply a place for family caregivers to get educated, empowered and energized. If you find
yourself feeling hopeless, exhausted and overwhelmed, let us offer some light and help shoulder the load. We hope you can take a deep breath knowing that you are not alone. Read more
Leeza’s Place Caregiver Support Blog
Medicare (United States)
Wikipedia
Medicare is a social insurance program administered by the United States government, providing health insurance coverage to people who are aged 65 and over; to those who
are under 65 and are permanently physically disabled or who have a congenital physical disability; or to those who meet other special criteria. Medicare in the United States somewhat resembles a
single-payer health care system, but is not. "Original Medicare" plans (when Medicare Advantage has not been elected) cover 80% of the Medicare-approved amount of any given medical cost; the
remaining 20% of cost must be paid by either a Medicare Supplement plan, which is a "supplemental insurance" from a private health insurance company (normally requiring a monthly insurance premium
paid to that company by the holder), or out-of-pocket via the patient's own personal funds (check, money order, cash, etc.). Medicare Advantage plans are not Medicare Supplements, but take the place
of "Original Medicare". In return for a premium, these plans share costs and cap out of pocket expenses.
The Medicare program also funds residency training programs for the vast majority of physicians in the United States.
The Social Security Act of 1965 was signed into law on July 30, 1965, by President Lyndon B. Johnson as amendments to existing Social Security legislation. This
legislation included the establishing of the Medicare program. At the bill-signing ceremony, Johnson enrolled former President Harry S. Truman as the first Medicare beneficiary and presented him with
the first Medicare card, and Truman's wife Bess, the second. Read more
................................Medicare Publications................................
Medicare has a number of publications that can provide important information for the care of a loved one. Here are some of the Medicare publications available online. These publications are also listed here in PDF format to download.
Medicare and Home Health Care
Medicare publication
Medicare and Home Health Care, 10969.pdf
Adobe Acrobat document [647.0 KB]
Medicare Guide to Choosing a Nursing Home
Medicare Guide to Choosing a Nursing Hom[...]
Adobe Acrobat document [951.5 KB]
Medicare Coverage of Skilled Nursing Facility Care
Medicare Coverage of Skilled Nursing Fac[...]
Adobe Acrobat document [383.6 KB]
Medicare Hospice Benefits
Medicare publication
Medicare Hospice Benefits, 02154.pdf
Adobe Acrobat document [392.8 KB]
Medicare Hospice Benefits, LARGE PRINT EDITION
Medicare Hospice Benefits, Large Print ([...]
Adobe Acrobat document [288.9 KB]
Tips for Caregivers of People with Alzheimer’s Disease, National Institute on Aging
National Institute on Aging, caregiving tip sheets and resources
Tips for Caregivers of People with Alzheimer’s Disease
NIA, National Institute on Aging, Caregi[...]
Adobe Acrobat document [287.6 KB]
Medicare Nursing Home Compare Tool
Medicare has an online Nursing Home Compare Tool that lets you compare several nursing homes. This tool rates nursing homes and locates specialized facilities such as a nursing home dedicated to caring for Alzheimer’s patients.
Medicare Guide to Choosing a Nursing Hom[...]
Adobe Acrobat document [156.1 KB]
Medicare Comprehensive Care Plan, 42 CFR §483.20
If your loved one enters a nursing home, a comprehensive care plan can improve the quality of their life. Medicare regulations require that residents entering a nursing home have a comprehensive care plan pursuant to 42 CFR §483.20. Medicare also requires an initial comprehensive assessment of each resident's functional capacity within 14 days of admission to a nursing home pursuant to 42 CFR §483.20. The Medicare publication "Guide to Choosing a Nursing Home" is very clear that the patient or family should be involved in the development of the plan, and have a copy of the plan.
Please see the following information about the care plan from the Medicare publication "Guide to Choosing a Nursing
Home":
Page 27: Will you be included in planning your care? Will your interests and preferences be included in the care plan? Will you be able to change the plan if you feel there is a need? Will you be
able to choose which of your family member or friends will be involved in the planning process? Will you get a copy of your care plan?
Page 47: Care Plans. The nursing home staff will get your health information and review your health condition to prepare your care plan. You (if you are able) or your family with your permission, or
someone acting on your behalf, have the right to take part in planning your care together with the nursing home staff.
Your care plan is very important. A good care plan can help make sure that you are getting the care you need and help make your stay more pleasant. Your health assessment (a review of your health
condition) begins on the day you are admitted. A comprehensive assessment must be completed within 14 days of admission. You should expect to get a health assessment at least every 90 days after your
first review, and possibly more often if your medical status changes.
Page 52: You have the right to take part in developing your care plan. You can also express any grievances you may have about your care and treatment. You also have the right to create an advance
directive.
Page 54: By law, nursing homes must develop a plan of care (care plan) for each resident. You have the right to take part in this process, and family members can help with your care plan with your
permission. If your relative is your legal guardian, he or she has the right to look at all medical records about you and make important decisions on your behalf.
The Law Firm of Motley Rice LLC
Federal Regulations and Nursing Homes
Patient Rights and Nursing Homes
All nursing home residents have rights protected by the Nursing Home Reform Act and Americans with Disabilities Act. In evaluating health care providers, you should be
aware of these rights to monitor care provided in a nursing home.
See Me - This poem was found among the possessions of an elderly lady who died in the geriatric ward of a hospital. No information is available concerning her -- who she was or when she died. Reprinted from the "Assessment and Alternatives Help Guide" prepared by the Colorado Foundation for Medical Care.
See Me
What do you see, nurses, what do you see?
 Are you thinking, when you look at me
--
Are you thinking, when you look at me
--
A crabby old woman, not very wise,
 Uncertain of habit, with far-away eyes,
Uncertain of habit, with far-away eyes,
Who dribbles her food and makes no reply,
 When you say in a loud voice -- "I do wish you'd
try."
When you say in a loud voice -- "I do wish you'd
try."
![]() Who seems not to notice the things that you do,
Who seems not to notice the things that you do,
 And forever is losing a stocking or shoe,
And forever is losing a stocking or shoe,
Who unresisting or not, lets you do as you will,
 With bathing and feeding, the long day to
fill.
With bathing and feeding, the long day to
fill.
![]() Is that what you're thinking, is that what you see?
Is that what you're thinking, is that what you see?
 Then open your eyes, nurse, you're looking at
ME...
Then open your eyes, nurse, you're looking at
ME...
I'll tell you who I am, as I sit here so still;
 As I rise at your bidding, as I eat at your
will.
As I rise at your bidding, as I eat at your
will.
I'm a small child of ten with a father and mother,
 Brothers and sisters, who
love one another,
Brothers and sisters, who
love one another,
A young girl of sixteen with wings on her feet.
 Dreaming that soon now a
lover she'll meet;
Dreaming that soon now a
lover she'll meet;
A bride soon at twenty -- my heart gives a leap,
 Remembering the vows that I
promised to keep;
Remembering the vows that I
promised to keep;
At twenty-five now I have young of my own,
 Who need me to build a
secure, happy home;
Who need me to build a
secure, happy home;
A woman of thirty, my young now grow fast,
 Bound to each other with ties
that should last;
Bound to each other with ties
that should last;
At forty, my young sons have grown and are gone,
 But my man's beside me to see
I don't mourn;
But my man's beside me to see
I don't mourn;
At fifty once more babies play 'round my knee,
 Again we know children, my
loved one and me.
Again we know children, my
loved one and me.
Dark days are upon me, my husband is dead,
 I look at the future, I
shudder with dread,
I look at the future, I
shudder with dread,
For my young are all rearing young of their own,
 And I think of the years
and the love that I've known;
And I think of the years
and the love that I've known;
I'm an old woman now and nature is cruel --
 'Tis her jest to make
old age look like a fool.
'Tis her jest to make
old age look like a fool.
The body is crumbled, grace and vigor depart,
 There is now a stone where
once I had a heart,
There is now a stone where
once I had a heart,
But inside this old carcass a young girl still dwells,
 And now and again my battered
heart swells.
And now and again my battered
heart swells.
![]() I remember the joys, I remember the pain,
I remember the joys, I remember the pain,
 And I'm loving and living
life over again,
And I'm loving and living
life over again,
I think of the years, all too few -- gone too fast,
 And accept the stark
fact that nothing can last --
And accept the stark
fact that nothing can last --
So I open your eyes, nurses, open and see,
 Not a crabby old woman,
look closer, nurses -- see ME!
Not a crabby old woman,
look closer, nurses -- see ME!
Authorized Electronic Monitoring (AEM) - Granny Cams
The state of Texas allows the family or guardian of a resident in a nursing home to monitor their loved one via a webcam, video surveillance camera, or similar device. It's called Authorized Electronic Monitoring (AEM) and is authorized under Subchapter R, Chapter 242, Health and Safety Code.
A facility must permit lawful monitoring per Texas Administrative Code
Texas Statutes - Subchapter R: Electronic Monitoring of Room
Texas DHS Information Regarding Authoriz[...]
Adobe Acrobat document [248.1 KB]
Request for Authorized Electronic Monito[...]
Adobe Acrobat document [30.5 KB]
Rule 92.129, Authorized Electronic Monit[...]
Adobe Acrobat document [38.5 KB]
Watchful Eye in Nursing Homes - New York Times
'Granny cam' law aimed at curbing nursing home abuse takes effect in Oklahoma, ABA Journal Law News Now
Watchful Eye in Nursing Homes
By Jan Hoffman, NYTNovember 18, 2013
Watchful Eye in Nursing Homes, The New York Times
A pretty nightie, a new lipstick, a fresh toothbrush: Doris Racher noticed that small things she had bought for her 96-year-old mother, Eryetha Mayberry, a dementia patient at a nursing home in Oklahoma City, had been disappearing. Ms. Racher assumed the culprit was another resident who sometimes wandered into her mother’s room and fell asleep in her bed.
So in 2012, Ms. Racher placed a motion-activated camera in her mother’s room. It looked like an alarm clock, and Ms. Racher nearly forgot about it.
About two months later, the family decided to pore through the recordings.
The camera had not caught the petty thief. But it captured something else:
An aide stuffed latex gloves into Mrs. Mayberry’s mouth, while another taunted her, tapping her on the head, laughing. Hoisting her from her wheelchair, they flung her on a bed. One performed a few heavy-handed chest compressions.
“My niece started bawling and couldn’t watch anymore,” said Ms. Racher, 78. “I was furious.” Mrs. Mayberry died soon after.
On Nov. 1, propelled by the outcry over the Mayberry case, Oklahoma became the third state — along with New Mexico and Texas — to explicitly permit residents in long-term care facilities to maintain surveillance cameras in their rooms. In the last two years, at least five states have considered similar legislation.
Although some states have administrative guidelines for electronic monitoring, most legislative efforts have stalled because of questions about liability and, in particular, privacy rights, raised by facility owners, unions, elder care lawyers and families. Read more
- Video Cameras Spreading in Nursing Homes to Prevent Abuse
- Is a Granny Cam a good way to monitor my elderly parents?
- Setting Up a Remote Web Cam
- All Eyes Are On Granny Cams
- Granny Cams
______________________________________
Aging In Place - Guide To Recognizing Elder Abuse
_______________________________________
Harvard Health Letter
Harvard Health Letter Volume 29, Number 9, 2004
Tip No. 8: Bring a tape recorder to your office visit. This may seem intrusive, but - especially if you have a serious medical condition like cancer or heart disease that involves complicated
treatment choices -listening to an audiotape after your visit may help you understand things you didn't grasp the first time around. Just refreshing your memory can be helpful. Canadian researchers
published a study of audiotaping visits last year in the Journal of Clinical Oncology. They found that breast cancer patients who listened to an audiotape of their first appointment about
chemotherapy had significantly better recall of having discussed the side effects than did patients who didn't listen to a tape.
Volume 29, Number 9, July, 2004
Harvard Health Letter, July 2004, Vol 29[...]
Adobe Acrobat document [182.2 KB]
CBS News
July 18, 2010
In the future, you may not have to go far to care for aging loved ones. Whit Johnson has a first look at the MedCottage which could be a new option for caring for the elderly in your backyard.
Read more
Americans For Stable Quality Care watch on YouTube
Aging with Dignity - Five Wishes End of Life Documents
Aging with Dignity is a national non-profit organization with a mission to affirm and safeguard the human dignity of individuals as they age and to promote better care for those near the end of life. The life and work of Mother Teresa of Calcutta served as the inspirational foundation of Aging with Dignity. Aging with Dignity founder Jim Towey served as Mother Teresa's friend and legal counsel for 12 years and was a full-time volunteer in her home for people with AIDS. Her tender care and concern for all a person’s needs – medical, emotional and spiritual – served as the inspiration for Five Wishes, America’s most popular living will.
Alzheimer’s related books
Joanne Koenig Coste, Author
After a major stroke left her husband paralyzed, unable to speak, and with significant progressive memory loss, Coste became his caregiver while raising four children.
Refusing to institutionalize him, she developed a humanistic approach to caregiving ("habilitation") that focuses on enhancing the individual's remaining functional, intellectual, emotional, and
spiritual abilities by creating a positive atmosphere that promotes feelings of success. Key elements of Coste's approach include simplifying the environment for the patient, capitalizing on his or
her remaining skills, and making an effort to understand what life must be like for the memory impaired. Read more
Authors Nancy L. Mace, MA and
Peter V. Rabins, MD, MPH
First published in 1981, The 36-Hour Day follows the format of the previous two editions but has been thoroughly updated to incorporate new information on the latest research, several drugs that hold
promise, and genetic aspects of Alzheimer's. The heart of the guide remains unchanged, focusing on helping families cope with this progressive and irreversible disease. Besides tips on how to care
for the demented during the various stages of the disease. Read more
Failure Free Activities for the
Alzheimer's Patient
Carmel Sheridan, Author
For so many victims of Alzheimer's disease, failure fills their days. Now caregivers of Alzheimer's patients can turn to this resource for ideas and advice for safe, reassuring activities to help the
patient feel capable and involved with everyday life. Adapted to suit the needs and capacities of the person with memory loss, the activities are designed to raise self-esteem, relieve boredom,
reduce feelings of isolation, develop and use remaining skills, promote involvement with reality, and emphasize abilities that remain. Read more
Failure Proof Activities, Dementia Today
A Caregiver's Guide to Alzheimer's Disease
Patricia R. Callone, Author
Winner of the 2006 American Journal of Nursing Book of Year Award, A Caregiver's Guide to Alzheimer's Disease will help readers understand what is physically happening to the brain so they can
empower their own special skills and talents throughout the disease process. Chapters cover legal and financial issues, family forums in the caregiving process, the role of medication at various
stages of the disease, helping children understand what is happening to a loved one, handling the holidays and celebrations, and making the living environment more stimulating and enjoyable. With an
abundance of pointers and guidelines for affected individuals, their families, friends and caregivers, A Caregiver's Guide to Alzheimer's Disease is essential for all readers who want to focus on the
capabilities that remain instead of those that have been lost. Read more
Never Say Die: The Myth and Marketing of the New Old Age
Susan Jacoby, Author
As the older members of the baby boom generation approach 65, marketers are at the ready with an abundance of "age defying" products and services. But is aging as trouble free as marketers tout and
aging consumers would like to believe? For her part, journalist Jacoby, herself in her 60s, admits to rage at the efforts to redefine old age without facing up to the unavoidable realities. For
example, after age 65, the prevalence of Alzheimer’s doubles every five years. She focuses on distinctions between the young old (60s and 70s) and the old old (80s, 90s, and the few 100s) as well as
the very different prospects for the elderly who are poor or minorities. Jacoby explores social, cultural, economic, and political changes in the concept of old age, from passage of the Social
Security Act to extended life expectancy and retirement, from the activism of the Gray Panthers to the ravages of Alzheimer’s. Drawing on research, personal experience, and anecdotes, she offers an
important reality check for Americans enamored of the images of healthy, active seniors featured in advertisements. - Vanessa Bush. Read
more
Book review, New York Times
The 10 Best Questions for Living with Alzheimer's
Dede Bonner, Ph.D., Author
The 10 Best Questions for Living with Alzheimer's is a guide you'll take with you to your doctor's office and keep close at hand as your loved one progresses from the initial diagnosis through all
the stages of the disease. In addition to the medical questions, you'll also learn what you need to ask your spouse or parent; questions to assess home safety issues, driving skills, and home care;
and how to care for your own emotional, legal, and financial health. more
On Death and Dying
Elisabeth Kubler-Ross, M.D., author
One of the most famous psychological studies of the late twentieth century, On Death and Dying grew out of an interdisciplinary seminar on death,
originated and conducted by Dr. Elisabeth Kübler-Ross. In On Death and Dying, Dr. Kübler-Ross first introduced and explored the now-famous idea of the five stages of dealing with death: denial and
isolation, anger, bargaining, depression, and acceptance. With sample interviews and conversations, she gives the reader a better understanding of how imminent death affects the patient, the
professionals who serve the patient, and the patient's family, bringing hope, solace, and peace of mind to all involved. Read more
Author interview, On Death and Dying
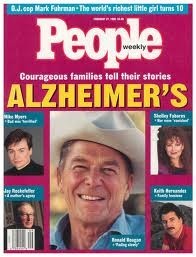
Alzheimer’s can strike anyone, even the President
The Vanishing President
People Magazine
Cover Story, Vol. 43, No. 8
February 27, 1995
Overtaken by Alzheimer's, Former President Ronald Reagan Joins Millions of Other Americans Struggling with the Disease That Devastates Families
LIKE AN ACTOR SETTLED INTO A LONG-RUNNING show, he continues to play the familiar role almost by rote: chopping wood, riding horses, visiting his office where, these days, the only business that
awaits are letters from well-wishers and a jar of jelly beans. But nearly four months after his poignant handwritten note informing the world that he was suffering from Alzheimer's disease, former
President Ronald Reagan, 84, is increasingly forgetting his lines and missing his cues. "About six months ago, he stopped recognizing me," Reagan's biographer, Edmund Morris, wrote recently. "Now I
no longer recognize him."
Reagan's November announcement dramatically focused attention on this incurable brain disease that now touches some 4 million Americans and kills 100,000 of them annually. With the U.S. population
gradually aging—the percentage of Americans over 85 has doubled in the past two decades—that figure is sure to grow. During the illness's relentless advance, patients suffer a host of symptoms that
destroy the very core of their being: memory loss, disorientation, personality changes. The cost of this disease to society is estimated at $100 billion a year, and that sum seems quite in proportion
to the illness's emotional toll. The disease can often be as devastating to the friends and families of Alzheimer's patients as to the victims themselves (see stories on following
pages).
Reagan's family began to notice his increasing disorientation in the year and a half before his announcement. Now his memory lapses are becoming more pronounced.
"He'll be in the middle of a story and forget the story," says a longtime friend of the man once known as the Great Communicator. "That exasperates him terribly."
He's "a vibrant guy who's not so vibrant anymore," admits Michael Reagan, 49, Reagan's son with first wife Jane Wyman. "Some days are better than others." Routine is important to Alzheimer's
patients, and on good days the ex-President's is the same as it has been since he left office. Accompanied by Secret Service agents, he is driven the 10 minutes from the couple's home in Bel Air to
his 34th-floor office in L.A.'s Century City. At his desk, Reagan reads his mail and receives old friends like actor Charlton Heston and multimillionaire Walter Annenberg before heading home around 3
p.m.
The former President works out daily with his personal trainer. Occasionally he sees close friends at small dinner parties, but he has stopped attending public functions. "In the early stages of the
disease, which is where Ronnie is, the Alzheimer's victim gets confused around unfamiliar people and surroundings," a friend explains. "Nancy has talked to experts and to friends whose husbands also
have Alzheimer's. She knows what to expect and how to handle Ronnie's illness." Five to seven days each month, the couple are at Reagan's beloved 688-acre ranch north of Santa Barbara. "Ronnie looks
forward more to the ranch than anything I know," says another friend.
Just a few short years ago, the former First Couple seemed on the cusp of a golden retirement. After leaving office, Reagan was inundated with lucrative offers for public appearances, acting jobs and
book deals. He took a 1989 trip to Tokyo, earning $2 million for two 20-minute speeches and some public appearances. In September 1990 he made an emotional visit to the remnants of the Berlin Wall,
and in November 1991 the four other U.S. Presidents living at the time gathered to honor him at the dedication of his presidential library in Simi Valley, Calif. But during the past two years his
appearances dwindled. "He was fading slowly," said biographer Morris.
Reagan's family can expect an increasing burden as his illness progresses, experts say. Although the entire clan, including formerly estranged daughter Patti, has rallied round and spent the holidays together, the heaviest load will fall on Nancy's slender shoulders. The former President, whose mother, Nelle, is thought to have suffered from Alzheimer's, touchingly alluded to his wife in his letter. "I only wish there was some way I could spare Nancy from this painful experience," he wrote. So far, though, "she is perfectly content riding on a slower trail with her husband," says her aide Cathy Busch. But "it's tough," acknowledges her stepson Michael. "It's hard to see someone you're in love with that much failing."
Ronald Reagan Alzheimer’s Letter, November 5, 1994
Former President Ronald Reagan joined millions of other Americans struggling with the disease that devastates families.
Ronald Reagan, Wikipedia
Ronald Reagan Alzheimer’s
letter November 5, 1994
November 5, 1994
Reagan's Alzheimer's letter.pdf
Adobe Acrobat document [23.9 KB]
The Vanishing Mind Series
Dementia Behind Bars: Dementia is a fast-growing phenomenon in prisons that many are not prepared to handle. The California Men’s Colony is using convicted killers to
care for inmates who can no longer care for themselves.
______________________________________
Aging In Place - Guide To Recognizing Elder Abuse
_______________________________________
Life, With Dementia
The New York Times
By PAM BELLUCK
February 25, 2012
SAN LUIS OBISPO, Calif. — Secel Montgomery Sr. stabbed a woman in the stomach, chest and throat so fiercely that he lost count of the wounds he inflicted. In the nearly
25 years he has been serving a life sentence, he has gotten into fights, threatened a prison official and been caught with marijuana.
Despite that, he has recently been entrusted with an extraordinary responsibility. He and other convicted killers at the California Men’s Colony help care for prisoners
with Alzheimer’s disease and other types of dementia, assisting ailing inmates with the most intimate tasks: showering, shaving, applying deodorant, even changing adult diapers. Read more
Finding Joy in Alzheimer’s
The New York Times
By ROBERT LELEUX
February 16, 2012
Seven years ago, when my grandmother JoAnn was first diagnosed with Alzheimer’s, the news sent me into a tailspin of fear and sadness.
In my splintered Southern family, JoAnn had been more than my grandmother. The Auntie Mame of my Texas childhood, she taught me that happiness requires a great deal of
thumbing one’s nose at convention. When I was 4, during an afternoon trip to the art museum, she told me to run my fingers along the brushstrokes of a particularly stunning Van Gogh: "They may kick
us out of here, darlin,’ " she drawled into my impressionable little ear, "but you’ll never not have touched that painting." It was a life-affirming, if inappropriate, lesson.
Without JoAnn’s outrageous example, I’m not sure I’d have had the courage to move to Manhattan, to come out of the closet, or ironically, to accompany her through the
final years of her life.
Little did I know that even after she was diagnosed with Alzheimer’s, my grandmother had only begun to educate me.
"The wonderful thing about Alzheimer’s," she once quipped after her diagnosis, "is that you always live in the moment."
This was a zinger intended to conceal her frustration at having forgotten the punch line to one of her signature anecdotes. But it was, nevertheless, quite true. Through
the haze of our grief, my grandfather Alfred and I began noticing that, along with her memories, JoAnn’s grudges, hurt feelings, worries and regrets were disappearing. In fact, within a year, she
seemed happier than ever, more present and at peace. Read more
Over 100 comments to this story.